Wills Eye Global Volunteer – Janice Gault, MD
By
 In May 2019, I spent a week in clinic teaching the first class of ophthalmology residents in Rwanda at RIIO, The Rwanda International Institute of Ophthalmology. The students had just finished their round of tests and were ready for the next step. It was quite a flashback—the first day they struggled to put drops in the patient's' eyes, check pressures and see the most basic things in the anterior segment through the slit lamp. I spent my evenings putting together presentations to reinforce the clinical applications they learned the day before. But, by the end of the week, they had learned a lot and so did I. Kigali is an amazing, bustling city, and it is completely safe. Interesting restaurants, art galleries and shops are everywhere. The country has come an incredible way from the genocide we all know about 25 years ago. Signs hang everywhere proclaiming “Kwibuka25—Remember-Unite-Renew”. It is a place of great hope. With this class of four residents and the six in the second class that started in July, Africa will have more home grown ophthalmologists that are desperately needed. Prior to this program, medical school graduates had to go abroad to be trained which meant that few of them returned to Kigali or Rwanda to work. In return for funding their training, the government is requiring the graduates to work in parts of Rwanda for several years where the need is greatest.
In May 2019, I spent a week in clinic teaching the first class of ophthalmology residents in Rwanda at RIIO, The Rwanda International Institute of Ophthalmology. The students had just finished their round of tests and were ready for the next step. It was quite a flashback—the first day they struggled to put drops in the patient's' eyes, check pressures and see the most basic things in the anterior segment through the slit lamp. I spent my evenings putting together presentations to reinforce the clinical applications they learned the day before. But, by the end of the week, they had learned a lot and so did I. Kigali is an amazing, bustling city, and it is completely safe. Interesting restaurants, art galleries and shops are everywhere. The country has come an incredible way from the genocide we all know about 25 years ago. Signs hang everywhere proclaiming “Kwibuka25—Remember-Unite-Renew”. It is a place of great hope. With this class of four residents and the six in the second class that started in July, Africa will have more home grown ophthalmologists that are desperately needed. Prior to this program, medical school graduates had to go abroad to be trained which meant that few of them returned to Kigali or Rwanda to work. In return for funding their training, the government is requiring the graduates to work in parts of Rwanda for several years where the need is greatest.
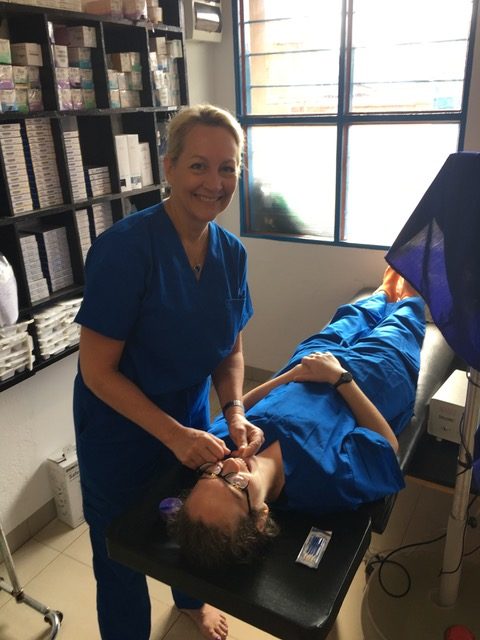
Two months after my trip to Rwanda I was back in Africa. This time I traveled to Burundi to work with John Cropsey and his team at Kibuye Hope Hospital. Although it’s only a short flight from Kigali to Burundi, they are on opposite extremes. Rwanda is growing economically with lots of cranes and construction across Kigali, and electricity and running water moving further and further out into the rural areas. Burundi is a very poor country. Eighty percent of people are subsistence farmers and much of the population suffers from malnutrition. John is running a high quality ophthalmology clinic and surgery. He has trained his staff incredibly well. He has an eye care team made up of ophthalmologists, optometrists and nurses who keep the high volume of patients moving through clinics at a steady pace.
 Patients walked to clinic and waited in the outdoor waiting room until they were seen. Often, they had surgery that day or the next. Patients came into the OR, often with help, because they could not see. No anesthesia except for a retrobulbar block, though children have the opportunity for anesthesia provided by the hospital anesthesiologist. Patients did not move or complain. I was humbled learning MSICS with dull crescent knives and portable microscopes. The results the next day were jaw-dropping. Light perception to 20/30 with a quiet anterior segment. Patients went home with a couple of drops and returned a month later to have the second eye done. If they were from far away, they had bilateral surgery on the same day. The joy was infectious. And it made me wonder why we spend so much on each cataract surgery here with more and more expensive equipment with so much waste when John’s results are so good. His IOLs from India are only $8. But, his name is out there—he’s one of two ophthalmologists in the country doing this type of work. He had patients come from Tanzania, Uganda, and Oman to see him in the few days I was there.
Patients walked to clinic and waited in the outdoor waiting room until they were seen. Often, they had surgery that day or the next. Patients came into the OR, often with help, because they could not see. No anesthesia except for a retrobulbar block, though children have the opportunity for anesthesia provided by the hospital anesthesiologist. Patients did not move or complain. I was humbled learning MSICS with dull crescent knives and portable microscopes. The results the next day were jaw-dropping. Light perception to 20/30 with a quiet anterior segment. Patients went home with a couple of drops and returned a month later to have the second eye done. If they were from far away, they had bilateral surgery on the same day. The joy was infectious. And it made me wonder why we spend so much on each cataract surgery here with more and more expensive equipment with so much waste when John’s results are so good. His IOLs from India are only $8. But, his name is out there—he’s one of two ophthalmologists in the country doing this type of work. He had patients come from Tanzania, Uganda, and Oman to see him in the few days I was there.
Everything is reused until it falls apart—thus the dull crescent knives. Thank goodness he had them because the new ones from India were stuck in customs somewhere in Bujumbura. We were running out of viscoelastic so John was using an anterior chamber maintainer. No change of gown or gloves between cases. Alcohol is used to sterilize the gloves, microscope and any tubing we were reusing. His endophthalmitis rates are extremely low.
I was surprised to see how much diabetic retinopathy is in Burundi. Not so surprised by the amount of glaucoma, often very severe at a young age; sometimes made worse with topical steroids for the common vernal conjunctivitis. I saw two young women blind from glaucoma secondary to steroid response. You could see the patients with large orbital tumors waiting on the benches, identifiable because of the hoodies over their heads to hide their appearance. The tumors were unbelievable. John is doing exenterations, to try and save lives but to also allow these individuals to be accepted back into society again. Patients are no longer ostracized from the community when the tumor is gone.
John has a Burundian ophthalmologist who recently trained abroad who has joined the team—and coincidently, he’s from the local town. John has also sent another ophthalmologist to Bangladesh to train in retina and another student is in the second ophthalmology residency class in Rwanda. He is planning for the future! He has great plans to resume the retinoblastoma program when his retina specialist returns. He has big plans for a large eye center—blueprints completed and land identified. Don’t be surprised to see him in the future to show you in person. The vision is incredible and there is no doubt it will come to fruition with him at the helm. Overall, my experience was so terrific, my husband, Jim Vander, is going in February to do some retina. More details to follow in the next issue! I’m excited to return.
Janice Gault, MD is a member of the Wills Eye Cataract & Primary Eye Care Service.
